Prisoners with Hepatitis C Can't Get Expensive Drug that Actually Works
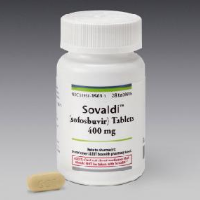
Around 17,000 California prison inmates have debilitating and deadly Hepatitis C, which until recently was extremely hard to treat. But a new wonder drug, Sovaldi, has hit the market and one pill a day for 12 weeks puts an end to most of the suffering.
However, it's doubtful very many people serving time are going to get it.
The drug costs $1,000 a day, or $84,000 for a full regimen of treatment for a single patient. That works out to $1.43 billion if administered to all infected state prisoners. A study out of Stanford University says that might be a reasonable price to pay, considering the longterm cost of administering less effective drugs. But corrections officials, and probably a lot of taxpayers, say that's not going to happen
Fewer than 1% of California's infected inmates (146) are receiving Sovaldi, made by Gilead Sciences of Foster City, which went on the market last December. It is one of four new Hepatitis C drugs approved by the Food and Drug Administration (FDA) in 2011 and is generally reserved for inmates with advanced stages of the disease.
The drug is an alternative to the 48-week, two-drug treatment that has miserable side effects and works about half the time. Sovaldi's cure rate is said to be 80-90% with fewer side effects.
The Stanford study said the big savings are in health costs down the line. Hepatitis C can cause catastrophic debilitation, including liver failure, that costs a lot of money to treat. “The health gains represent good value for the money,” Jeremy Goldhaber-Fiebert, an assistant professor at the Stanford School of Medicine and the study's senior author, told the San Francisco Business Times.
If inmates were treated with Sovaldi, the cost would be picked up by the Corrections department, but the financial benefits would accrue to federal Medicaid and other insurers and hospitals after the prisoner is released. That is just one of the stumbling blocks for policymakers.
Around 15,000 Americans die annually of Hepatitis C out of the 3.2 million afflicted with the disease. Around 500,000 infected people are sitting in U.S. prisons. Stanford's researchers calculated that the new drugs could save $2 billion to $5 billion by preventing the need for expensive liver cancer treatment and liver transplants. But its numbers could be skewed if patients continue to re-infect themselves, the study said. Hepatitis C in the U.S. is most often spread through the sharing of drug-injection needles, but it passes via blood and can be transmitted by toothbrushes, razors or rough sex.
Despite a blizzard of stories in the media about the new Hepatitis C drugs and their costs, there is little discussion about the cost-analysis justification for the high prices. A U.S. Senate Finance Committee asked Gilead CEO John Martin in July to explain whether “the market for this drug is operating efficiently and rationally.” The request was in writing and the answer unknown.
The Wall Street Journal's Pharmalot blog wasn't too optimistic that congressional investigations are going to have much of an effect on drug prices. The U.S., unlike European governments, does not bargain much with Big Pharma.
The blog quoted Wells Fargo Securities analyst Brian Abrahams calling the letter from the senators “more noise.” Abrahams wrote, “Based on our checks, we do not expect this will translate to any significant legislative action on pricing for Sovaldi (or other drugs).”
–Ken Broder
To Learn More:
Prisons Balk at Sovaldi’s $84,000 Cost for Hepatitis C Treatment (by Stephanie M. Lee and Joe Garofoli, San Francisco Chronicle)
Gilead's $1,000-a-Pill Hepatitis C Drug May Make Financial Sense for Prisons (by Ron Leuty, San Francisco Business Times)
For Inmates, Pricey Hepatitis C Drug Could Make Financial Sense (Stanford Medicine News Center)
Senate Lawmaker Eyes Hearing on the Cost of Hepatitis C Treatments (by Ed Silverman, Wall Street Journal)
Expensive New Hepatitis C Medicine, Seen as Harbinger of Specialty Drugs to Come, Poses Challenge to Health Care System (by Noel Brinkerhoff and Steve Straehley, AllGov)
Sofosbuvir-Based Treatment Regimens for Chronic, Genotype 1 Hepatitis C Virus Infection in U.S. Incarcerated Populations: A Cost-Effectiveness Analysis (by Shan Liu, Daena Watcha, Mark Holodniy, and Jeremy D. Goldhaber-Fiebert, Annals of Internal Medicine)
- Top Stories
- Controversies
- Where is the Money Going?
- California and the Nation
- Appointments and Resignations
- Unusual News
- Latest News
- California Forbids U.S. Immigration Agents from Pretending to be Police
- California Lawmakers Urged to Strip “Self-Dealing” Tax Board of Its Duties
- Big Oil’s Grip on California
- Santa Cruz Police See Homeland Security Betrayal in Use of Gang Roundup as Cover for Immigration Raid
- Oil Companies Face Deadline to Stop Polluting California Groundwater





