Women Told Not to Fear Long Childbirth Labor, but Question Mammograms
 (AP photo)
(AP photo)
Two new medical studies have given women plenty to think about regarding the benefits of mammograms and the point at which a doctor should intervene during lengthy childbirth.
On the subject of epidurals, researchers found that the use of that form of anesthesia, given during the second stage of labor (the time when the woman pushes), is associated with longer deliveries.
The study suggested a normal second stage can take as long as 5.6 hours for first-time mothers who get epidurals and as long as 3.3 hours for those who don’t get epidurals. Until now, it had been commonly believed that an epidural only added an hour’s difference. So doctors, thinking that something was going wrong with the birth, had been stepping in with interventions, when the effect of the epidural was simply lengthening the time of the second stage.
Hearing of these findings, some experts said doctors may want to adjust their approach to cutting labor short if the woman has had an epidural.
“Clinicians might need to wait later before intervening with oxytocin, forceps, vacuum or a cesarean,” Dr. S. Katherine Laughon, an investigator at the National Institutes of Health who was not involved in the study, told The New York Times.
It is important for physicians and patients to balance the “benefits of vaginal delivery with potential increases in risk for mom and baby,” said Dr. Laughon, who is also an obstetrician and gynecologist.
Another expert, Dr. Barbara Leighton, a professor of anesthesiology at Washington University School of Medicine in St. Louis, who has researched the effects of epidurals on labor, said: “One of the messages of this study is, sit on your hands a little longer, don’t rush into an instrumental vaginal delivery or a cesarean, because really everything could be fine.”
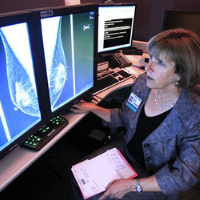
Meanwhile, a second medical report, which followed 90,000 Canadian women, raised serious questions about the value of getting mammograms.
It found that women between 40 and 59 who got mammography weren’t less likely to die of breast cancer than those who just got breast exams by doctors or trained nurses.
Also, about 20% of cancers discovered with mammography and treated were not a threat to the woman’s health and would not ordinarily require interventions such as chemotherapy, surgery or radiation, according to the study published in the British Medical Journal.
“It will make women uncomfortable, and they should be uncomfortable,” Dr. Russell P. Harris, a screening expert and professor of medicine at the University of North Carolina at Chapel Hill, who was not involved in the study, told the Times. “The decision to have a mammogram should not be a slam dunk.”
-Noel Brinkerhoff, Vicki Baker
To Learn More:
Vast Study Casts Doubts on Value of Mammograms (by Gina Kolata, New York Times)
Twenty Five Year Follow-up for Breast Cancer Incidence and Mortality of the Canadian National Breast Screening Study: Randomised Screening Trial (by Anthony B. Miller, Claus Wall, Cornelia J. Baines, Ping Sun, Teresa To, and Steven A. Narod; BMJ) (pdf)
Too Much Mammography (by Mette Kalager, Hans-Olov Adami, and Michael Bretthauer; BMJ)
Study Suggests Misplaced Fears in Longer Childbirths (by Catherine Saint Louis, New York Times)
Second Stage of Labor and Epidural Use: A Larger Effect Than Previously Suggested (by Yvonne W. Cheng, MD, PhD; Brian L. Shaffer, L. MD; James M. Nicholson, MD, MSCE; and Aaron B. Caughey, MD, PhD; Obstetrics & Gynecology) (abstract)
Report Points Finger at Doctors for Elective Surgery Choices being “All Over the Map” (by Ken Broder, AllGov California)
“Smart Bra” Is Years Faster than Mammograms in Detecting Breast Cancer (by Noel Brinkerhoff, AllGov)
Caesarean Births in U.S. Hit All-Time High (by Noel Brinkerhoff, AllGov)
- Top Stories
- Unusual News
- Where is the Money Going?
- Controversies
- U.S. and the World
- Appointments and Resignations
- Latest News
- Trump to Stop Deportations If…
- Trump Denounces World Series
- What If China Invaded the United States?
- Donald Trump Has a Mental Health Problem and It Has a Name
- Trump Goes on Renaming Frenzy






Comments